comprehensive
Previous article:
State Dept. review finds Biden bears some blame for Afghanistan failures
Next article: Malaysia cuts short music fest after British band slams anti
Next article: Malaysia cuts short music fest after British band slams anti
entertainment
Wikipedia
-
Biden administration sends mixed signals on US soldier who crossed into North Korea
2025-08-25 07:02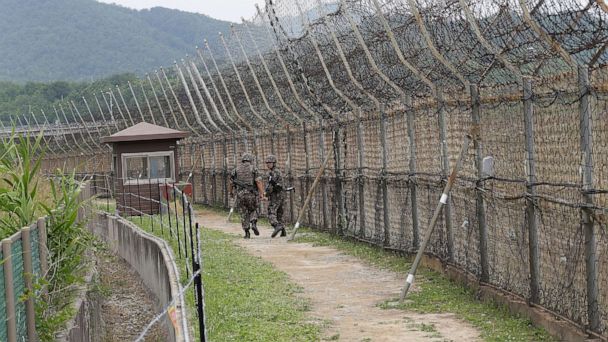
-
What we know about the American soldier detained in North Korea
2025-08-25 06:53
-
Burning questions about Delta and the next phase of the Covid pandemic
2025-08-25 06:48
-
Search resumes for 2 missing children washed away with mom in deadly Pennsylvania flash flood
2025-08-25 06:05
-
Flagship, Pfizer team up in deal worth up to $7 billion
2025-08-25 06:00
-
Transgender women dream of pregnancy via uterus transplants
2025-08-25 04:50

